This module is organized into four content sections. Each section includes a slide deck presentation. Additional links and resources are also provided. A complete reference list is included at the end of the module.
This section provides a discussion about urinary tract infections, definitions and signs/symptoms.
|
|
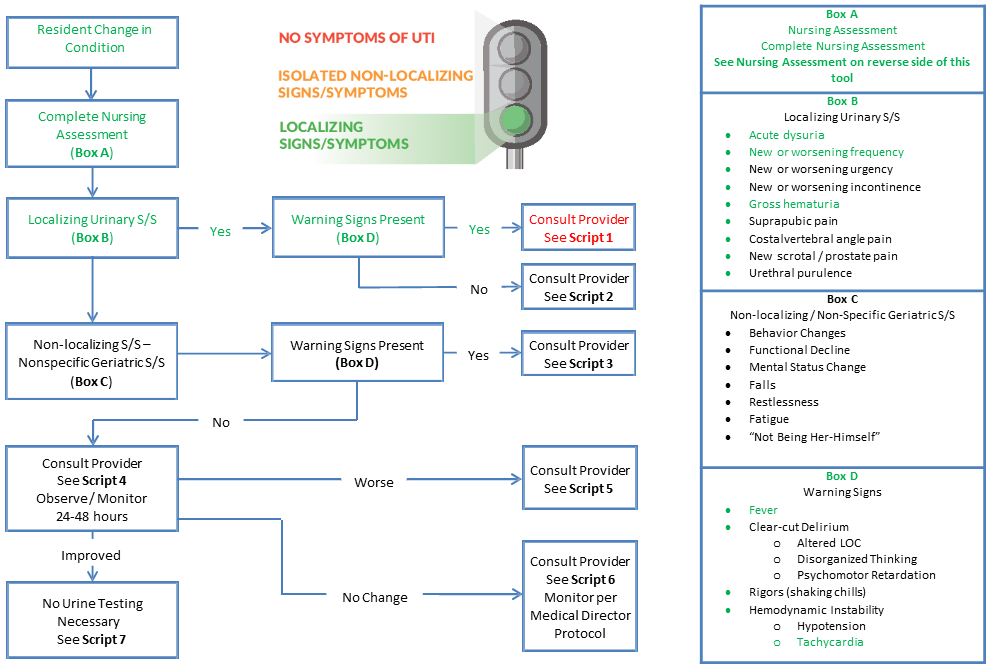
This section provides an instructive presentation for nursing home UTI management champions in preparation to educate staff, including an introduction to the UTI Stoplight Tool and When to Test Urine-Nursing Tool.
|
|
UTI Stoplight When to Test Nursing Tool Active Monitoring Tracking Form |
This section includes the application of the When to Test Urine-Nursing Tool to seven case studies. The first script scenario described is indexed to decision points on the When to Test Urine-Nursing Tool and includes suggestions for appropriate communication strategies. Six additional case studies and sample forms are provided, along with answer keys.
|
|
When to Test Nursing Tool Communication Script Template |
Situation: Jimmy has sudden onset of acute dysuria and frequency. Gross hematuria is present with small clots. There is no suprapubic or costovertebral tenderness.
Resident evaluation: He has mildly increased confusion since mid-afternoon today. He has had a functional decline requiring an increase in staff assist with bed mobility, transfers, and other ADLs. His appetite is diminished and oral fluid intake in the last 16hr is 600 CCs. Lungs are clear. Bowel sounds are present in all 4 quadrants. Abdomen is non-tender with no vomiting or diarrhea. His urine is dark colored and has mucous shreds.
Appearance: This resident is exhibiting localizing urinary tract signs and symptoms with hypoxia and warning signs of fever and tachycardia.
When to Test Nursing Tool 1
Physician Communication Script 1
This message is to inform you of a change in condition:
Chief Complaint: Acute onset of dysuria and fever over the last two hours.
Situation: Jimmy has sudden onset of acute dysuria and frequency. Gross hematuria is present with small clots. There is no suprapubic or costovertebral tenderness.
Resident evaluation: He has mildly increased confusion since mid-afternoon today. He has had a functional decline requiring an increase in staff assist with bed mobility, transfers, and other ADL's. His appetite is diminished and oral fluid intake in the last 16hr is 600 CCs. Lungs are clear. Bowel sounds are present in all 4 quadrants. Abdomen is non-tender with no vomiting or diarrhea. He has mucous shreds, urine is dark colored.
Appearance: This resident is exhibiting localizing urinary tract signs and symptoms with hypoxia and warning signs of fever, tachycardia.
Situation: Tommy has acute onset of dysuria, urgency and frequency with no costo-vertebral or suprapubic tenderness. Urine is clear and amber.
Resident evaluation: He has no recent med changes or change in mental status. His oral intake is unchanged, weight is stable, follows commands and is oriented in person, place, and time. He has no shortness of breath, chest or abdominal pain and he has not vomited. Bowel sounds are normal.
Appearance: The resident is exhibiting localizing signs and symptoms of a localized urinary tract infection without warning signs.
When to Test Nursing Tool 2

Physician Communication Script 2
This message is to inform you of a change in condition:
Chief Complaint: Acute onset of dysuria, urgency and frequency starting after lunch today.
Situation: Tommy is complaining of acute dysuria, urgency and frequency. He has been incontinent three times today which is unusual for him. Urine is clear and amber in color. He has no costovertebral angle tenderness or suprapubic tenderness. He is not otherwise in distress.
Resident evaluation: He's had no recent medication changes. He has no change in mental status and is oriented to person, place and time and follows commands. He is independent with ADLs. He's eating and drinking and is on a 1400 cc 24 hr. fluid restriction and took in 1400 ccs in the last 24 hours. His weight is stable. There is no shortness of breath, chest or abdominal pain and he is not vomiting. Bowel sounds are active in all quadrants.
Appearance: This resident is exhibiting localizing symptoms suggesting the need to obtain a urinalysis.
Situation: Larry is 6 days post-op Cholecystectomy with acute mental status changes with confusion, not feeling himself, poor appetite, without localizing urinary tract signs or symptoms.
Resident evaluation: He has no cough, diarrhea, vomiting, rash or skin sores. He denies dysuria, we see no urinary tract signs or symptoms. He has no history of diabetes or heart condition. But he does have a past history of alcohol abuse.
Appearance: This resident is post-op day 6. He has acute confusion with warning signs of fever and hypoxia. He has no localizing signs or symptoms of obvious infection. His blood sugars are elevated, but he has no prior history of diabetes mellitus.
When to Test Nursing Tool 3

Physician Communication Script 3
This message is to inform you of a change in condition:
Chief Complaint: Acute confusion with fever beginning at noon today and worsening through the day.
Situation: Larry is 71 y/o male six days post-op cholecystectomy who has a complaint of general discomfort. He has no site specific pain. He says, “I just don’t feel good. I want to go home.” He has had a mental status change of acute confusion with some lethargy but excitable and trying to go home. His appetite has been poor, he refused lunch today. He has been continent and independent of bowel and bladder since he arrived and he has no evidence of any localizing urinary symptoms.
Resident evaluation: There is no cough, vomiting, diarrhea, or rash or skin sores. He has no incontinence, denies dysuria and we see no localized signs or symptons of UTI. There is a past history of alcohol abuse. There is no prior history of diabetes or heart condition.
Appearance: This resident is post-op day 6. He has acute confusion with fever and hypoxia. He has no localizing signs or symptoms of obvious infection. His blood sugars are elevated, but he has no prior history of diabetes mellitus.
Situation: Suzi has mild generalized discomfort with mild confusion but orientable. She refused activities today and appetite is poor. She remains alert. She had recent med change with addition of gabapentin for chronic pain.
Resident evaluation: She's had no recent falls or exposure to infectious residents or visitors. Lungs are clear. She has no chest pain, no change in BMs, no vomiting or diarrhea, no skin rashes or sores, and no new joint, chest, or abdominal pains. There are no localizing urinary symptoms or signs.
Appearance: Suzi has 24-36 hrs. of poorly localized general discomfort with mild confusion and poor appetite without warning signs, localizing urinary or other focal S/Sx's.
When to Test Nursing Tool 4

Physician Communication Script 4
This message is to inform you of a change of condition:
Chief Complaint: Generalized discomfort and mild confusion since lunch today.
Situation: She has a complaint of generalized discomfort. She has had a mental status change of mild lethargy and mild confusion tending to wander but is orientable. She didn't go to activities this afternoon. Appetite poor since this morning. She remains alert. She has a recent med change consisting of addition of gabapentin 300 mg bid oral for pain.
Resident Evaluation: She has not recently fallen. There is no exposure to infectious residents or visitors. Lungs are clear and there is no chest pain. She has had no change in BMs with last one yesterday and there is no vomiting or diarrhea. There are no localizing urinary symptoms or signs. There are no skin rashes or sores, and no new joint, chest, or abdominal pains.
Appearance: This resident is an elderly female with 24-36 hours of complaint of poorly localized general discomfort with mild confusion and poor appetite. She has no warning signs, no localizing urinary signs or symptoms and no signs or symptoms of other focal infection.
Situation: Suzi has been on observation since 4:00PM yesterday for mild non-localized pain with poor appetite and mild confusion and lethargy. She has developed tachypnea with drop in O2 Sat while on room air. She has only eaten 10% in the last 24 hrs. with fluid intake of 400cc only.
Resident evaluation: Confusion is worse. Lungs are clear. There is no chest or abdominal pain, no bowel changes or vomiting, no rash or skin sores, and no localized urinary S/Sx's. She's had no exposure to infected residents or visitors.
Appearance: Suzi has new hypoxia and tachypnea while being observed 24-48 hrs. for the new complaint of generalized pain, poor appetite, mild confusion. She exhibits no urinary tract S/Sx's and no other focal evidence of infection.
When to Test Nursing Tool 5

Physician Communication Script 5
This message is to inform you of a change of condition:
Chief Complaint: Changing condition during 24 Hr. observation period now with tachypnea and hypoxia.
Situation: She has been on 24 Hr. observation since 4:00PM yesterday for increase of mild non-localized pain with poor appetite and mild lethargy. In past four hours has developed sustained rapid breathing and drop in O2 sat while on room air. She has only eaten 10% in the last 24 hrs. with fluid intake of 400cc only.
Background:
Resident evaluation: She remains alert but has difficulty focusing and is incoherent for brief periods. There has been no recent exposure to infectious residents or visitors. Lungs are clear and there is no chest pain. She had a normal bowel movement last night and there is no vomiting or diarrhea. There are no localizing urinary signs or symptoms, hematuria, abdominal or flank pain. There are no skin rashes or sores, and no new joint or abdominal pains.
Appearance: This resident is an elderly female who developed new tachypnea and hypoxia while she was undergoing a period of observation for the complaint of poorly localized general discomfort with mild confusion and poor appetite. She continues to show no signs or symptoms of focal infection and there are no localizing urinary tract signs or symptoms.
Situation: Suzi has been on 48 hr. observation for mild generalized pain, mild confusion, and recent med change with addition of gabapentin for chronic pain. These symptoms continue without change and no new findings including no S/Sx's of localized urinary tract findings.
Resident evaluation: She was observed and treated with prn acetaminophen. She has no change in symptoms. She is alert and oriented x3. Denies headache, dyspnea, chest pain, abd pain or dysuria, with normal bowel function. There is no rash or sores. Lungs clear. Abd soft.
Appearance: She has been on 48 hr. observation for mild increase of diffuse pain and mild confusion. She is no better. She has no localized urinary tract signs or symptoms or other S/S's of focal infection.
When to Test Nursing Tool 6

Physician Communication Script 6
This message is to inform you of a change of condition:
Chief Complaint: No improvement of pain, mild confusion and poor appetite after a 48 hr. period of observation that began on 10/21 at 4:00 PM.
Situation: She has been on 24-48 hr. observation for the complaint of generalized discomfort and mild confusion with recent addition of gabapentin to medication regimen. These symptoms have continued without improvement in spite of using prn acetaminophen, encouraging oral intake. She has had no worsening pain, no new significant complaints or signs or symptoms of other infection, other illness, and no localized urinary signs or symptoms.
Resident evaluation: She was observed and treated with prn acetaminophen according to standing orders. She continues with same complaints without increase of pain or confusion. She is alert and oriented x3. Denies headache, dyspnea, chest pain, abd pain or dysuria. She had a bowel movement yesterday with normal consistency. There is no rash or sores. Lungs clear.
Appearance: She has been on 48 hr observation for change of condition consisting of mild increase of diffuse pain and mild confusion. She is not better. She has no localized urinary tract signs or symptoms or other S/S's of focal infection.
Situation: She has been on 24-48 hrs. observation for generalized discomfort and mild confusion. She has returned to baseline with pain is improved with scheduled acetaminophen.
Resident evaluation: She had no new significant complaints or signs or symptoms of focal infection. She has continued on her regular medication including new gabapentin.
Appearance: She had no new complaints or signs or symptoms of localized infection or other illness. She was observed and treated according to standing orders. She has resumed normal activity and intake.
When to Test Nursing Tool 7

Physician Communication Script 7
This message is to inform you of outcome following 24 hr. skilled nurse observation for increased pain and mild confusion beginning 10/21/14 at 4:00PM
Chief Complaint: Symptoms resolved. Resident condition returns to baseline.
Situation: She has been on 24-48 hrs. of skilled nursing observation for the complaint of generalized discomfort and mild confusion. She has returned to baseline alertness, intake and activity and says her pain is improved with scheduled acetaminophen within limits of her current orders. She had no new significant complaints or signs or symptoms of focal infection. She has continued on her regular medication regimen including new gabapentin order from a week ago.
Appearance: She had no new significant complaints or signs or symptoms of localized infection or other illness. She was observed and treated according to standing orders. She has resumed normal activity and intake.
Familiarity with all aspects of the WI UTI Toolkit will allow you to effectively educate your staff and serve as a resource in your facility for questions from staff, administration, residents and their families regarding antibiotic stewardship. The following outline suggests a model for developing a staff educational plan to share information provided in the WI UTI Toolkit and encourages participation by staff in the antibiotic stewardship process.
The use of structured forms and tools may assist staff to standardize the assessment, communication and documentation process. Examples include the Agency for Health Services Research and Quality (AHRQ) and Optimizing Antibiotic Stewardship in Skilled Nursing Facilities (OASIS) tools targeted for cases of suspected UTI. The INTERACT form provides a more general framework for organizing and reporting resident information related to change in condition.